If you are one of the many who have suffered with chronic back pain, leg pain and numbness or weakness of the arms or legs, you many also have been told that the discs in your spine are to blame. When patients are first diagnosed with an intervertebral disc problem, (usually through diagnostic imaging) a common first reaction is one of confusion.
What is a disc?
How did this happen?
Why do I have leg/arm pain if the problem is in my back?
How do I fix this?
Perhaps you have heard of the term “pinched nerve” or “disc bulge” or even “slipped disc.” These are some of the names that can be used to describe a mechanical problem relating to the intervertebral discs.
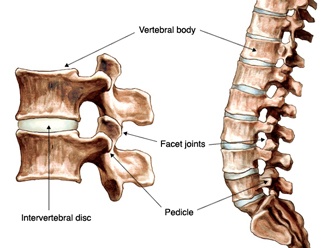
Before understanding the complexity of an intervertebral disc injury, it is important to know what a intervertebral disc is and what its main function is. Intervertebral discs have 3 main functions.
- They work to absorb the shock in between each vertebrae during impact or activity.
- They mimic ligaments in that they help maintain the alignment of the vertebra and spine in general.
- They work as flexible joints that allow for movement of the spine.
The intervertebral discs are made up of mainly water. The outer portions of intervertebral discs are made up of collagen fibers. Inside that shell of collagen is a gel-like substance. This allows for a better distribution of weight and pressure.
If the disc between two vertebrae is no longer aligned with the spinal column, this can be the result of a disc herniation, or a disc bulge. When the disc itself has changed in height, this can be due to disc degeneration.
Disc Herniation: While herniated disc can often be the result of an injury or strain in the spine, it can also occur as part of the normal aging process. A disc herniation refers to the gel like substance pouring out of the disc. This is usually the result of a crack or tear of the outer shell of the disk. When this happens, it is often not the disc itself that is painful, but rather the nerves that are in close proximity to the disc that are painful. The nerves for different levels of the spine tend to pass close by the intervertebral discs. Discs commonly herniate directly under the nerve root because of the anatomy of the spine. When the gel-like substance protrudes out of its original space, it can push up against the closest nerve, causing inflammation of the nerve, numbness and pain that radiates into the arms (if the disc herniation is in the cervical spine or neck) or into the legs (when the disc herniation is in the lumbar spine or back). While disc herniation in the thoracic spine are rare, they can happen.
When a herniated disc causes only leg pain or arm pain, the possibility that the root of the problem might be located in the spine is often overlooked by the patient and so they are surprised to find out that a herniated disc is the culprit.
Disc Bulge: Most intervertebral disc bulges go undetected because there are no symptoms. In fact, many people have a disc bulge and don’t even know it. A disc bulge becomes problematic when the bulge causes irritation to a nerve, or when the bulge or balloon ruptures (disc herniation) and the gel-like material seeps out, irritating nerves. A disc bulge can result from increased pressure on the intervertebral discs, or by the normal aging process. When the disc losses some of its water content, the disc can become more firm, flatter and lose its ability to recoil back to original shape. An increase in pressure can cause a part of the disc to balloon out in order to accommodate the increased pressure and because it is no longer able to recoil, the disc remains ballooned or bulged.
Disc Degeneration: Disc degeneration is a term used to describe the wearing down of the intervertebral discs in the spine. This can occur with age, or it can be accelerated by an acute injury, such as a fall that results in a disc herniation. Our bodies change with age or injury. The same can be said for the intervertebral discs. These changes include a loss of the fluid in the disc which can make the intervertebral discs harder, less flexible, and more prone to tears and cracks. A loss of fluid can also cause the vertrebral disc to become shorter, decreasing the space and cushioning between the vertebre. The changes happening in the disc space can lead to inflammation, and pain down the leg otherwise known as sciatica. Disc degeneration can also lead to instability of the spine since the intervertebral discs play an important role in the alignment of the spine. Many who are diagnosed with disc degeneration have also noted muscle spasms of the affected area.
The treatments for intervertebral disc conditions vary from person to person. Those who experience little to no symptoms may not require any further intervention. Those with mild symptoms can benefit from exercise and over the counter medications, provided they have been assessed by their primary care physician first. For those with moderate to severe symptoms such as chronic pain and ongoing weakness, talk to your doctor and discuss your treatment options. Interventions that are centered on chronic pain may be suitable for you. Prescribed medications and physiotherapy can also be beneficial. Sometimes, surgery is also an option if other treatments have been unsuccessful. Talk to your doctor to find out which treatments are best suited for you.